Protein OverloadMuscle, vitality,
strength, power, energy, vigor, aggressiveness, and liveliness are words
that come to mind when people think of the benefits of protein in their
diet. The truth is quite the opposite. Bone loss,
osteoporisis, kidney damage, kidney
stones, immune dysfunction, arthritis, cancer promotion, low-energy, and overall poor health are
the real consequences from overemphasizing protein. Protein serves as raw
material to build tissues. Without sufficient protein from your diet,
your body would be in trouble – but, aside from starvation, this never
happens. Yes, a little protein is good, but more is not better. Protein
consumed beyond our needs is a health hazard as devastating as excess
dietary fat and cholesterol. Unfortunately, almost everyone on the
typical Western diet is overburdened with protein to the point of physical
collapse. The public has almost no awareness of problems of protein
overload, but scientists have known about the damaging effects of excess
protein for more than a century.
In his book, Physiology Economy in
Nutrition, Russell Henry Chittenden, former
President of the American Physiological Society (APS) and Professor of
Physiological Chemistry at Yale, wrote in 1905, “Proteid (protein)
decomposition products are a constant menace to the well-being of the
body; any quantity of proteid or albuminous food beyond the real
requirements of the body may prove distinctly injurious…Further, it
requires no imagination to understand the constant strain upon the liver
and kidneys, to say nothing of the possible influence upon the central and
peripheral parts of the nervous system, by these nitrogenous waste
products which the body ordinarily gets rid of as speedily as possible.”1

What are
Your Construction (Protein) Needs?
Protein from
your diet is required to build new cells, synthesize hormones, and repair
damaged and worn out tissues. So how much do you need?
The protein lost from the body each day
from shedding skin, sloughing intestine, and other miscellaneous losses is
about 3 grams per day (0.05 grams/Kg).3 Add to this loss other
physiological requirements, such as growth and repairs. The final tally,
based on solid scientific research, is: your total daily need
for protein is about 20 to 30 grams.4,5 Plant
proteins easily meet these needs.6
So what are people consuming? Those
living in many rural Asian societies consume about 40 to 60 grams from their
diet of starch (mostly rice) with vegetables.6 On the Western diet,
typical food choices centered around meat and dairy products, “a
well-balanced diet,” provides about 100 to 160 grams of protein a day. A
traditional Eskimo, eating marine animals, or someone on the Atkins diet,
from various kinds of meat and dairy, might be consuming 200 to
400 grams a day.7 Notice that there
can be a 10-fold (1000%) difference from our basic requirements and the
amount some
people consume. The resilience of the human body allows for survival
under conditions of incredible over-consumption.

Once the body’s needs are
met, then the excess must be removed. The liver converts the excess
protein into urea and other nitrogen-containing breakdown products, which
are finally eliminated through the kidneys as part of the urine.

Excess Protein Burdens
the Kidneys and Liver
Processing all that excess dietary protein
– as much as 300 grams (10 ounces) a day –causes wear and tear on the
kidneys; and as a result, on average, 25% of kidney function is lost over
a lifetime (70 years) from consuming the Western diet.8,9 Fortunately, the
kidneys are built with large reserve capacity and the effects of losing
one-quarter of kidney function are of no consequence for otherwise healthy
people. However, people who
have already lost kidney function for other reasons – from an accident,
donation of a kidney, infection, diabetes, and hypertension – may suffer
life-threatening consequences from a diet no higher in protein than the
average American consumes.10,11
The time-honored fundamental treatment for
people with failing kidneys is a low-protein diet. End-stage kidney
failure, requiring dialysis, can usually be postponed or avoided by
patients fortunate enough to learn about the benefits of a low-protein
diet.10-13
People suffering with liver failure are also placed on diets low in
protein as fundamental therapy – short of a liver transplant, this is the most important therapy they
will receive. During the end stages of liver failure, patients will often
fall into a coma from the build-up of protein breakdown products (hepatic
coma). A change to a cost-free, very low-protein diet can cause these
dying people to awaken. Well planned, plant-food based diets are
particularly effective with both kidney and liver disease.14,15
Excess Protein Damages the Bones =
Osteoporosis
Worldwide, rates of hip fractures (and
kidney stones) increase with increasing animal protein consumption
(including dairy products). For example, people from the USA, Canada,
Norway, Sweden, Australia, and New Zealand have the highest rates of
osteoporosis. 15,16 The lowest rates are among people who eat
the fewest animal-derived foods (these people are also on lower calcium
diets) – like the people from rural Asia and rural Africa.15,16
Osteoporosis is caused by several
controllable factors; however, the most important one is the foods we
choose – especially the amount of animal protein and the foods high in
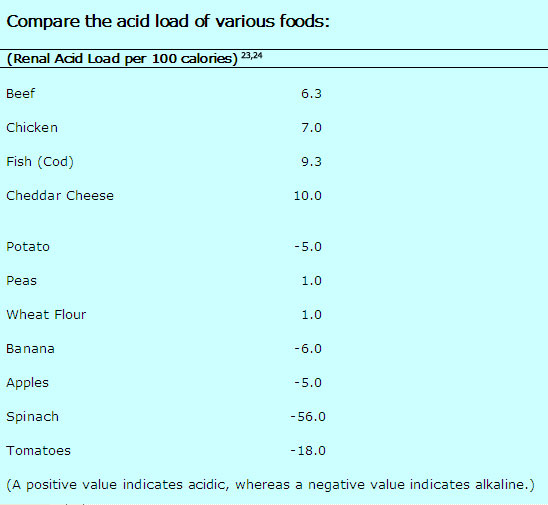
acid.17-19 The high acid foods are meat, poultry, fish,
seafood, and hard cheeses – parmesan cheese is the most acidic of all
foods commonly consumed.20 This acid must be neutralized
by the body.21 Carbonate, citrate and sodium are alkaline materials
released from the bones to neutralize the acids. Fruits and vegetables
are alkaline and as a result a diet high in these plant foods will
neutralize acid and preserve bones. The acidic condition of the body
caused by the Western diet also raises cortisol (steroid) levels. 22
Elevated cortisol causes severe chronic bone loss – just like giving
steroid medication for arthritis causes severe osteoporosis.
Consequence Two: Kidney Stones
Once materials are released from the solid bone, the
calcium and other bone substances move through the blood stream to the
kidneys where they are eliminated in the urine. In an effort to remove the
overabundance of waste protein, the flow of blood through the kidneys
(glomerular filtration rate) increases – the result: calcium is filtered
out of the body. Naturally, the kidneys attempt to return much of this
filtered calcium back to the body; unfortunately, the acid and
sulfur-containing amino acids from the animal foods thwart the body’s
attempts to conserve calcium. The final result is each 10 grams of
dietary protein in excess of our needs (30 grams daily) increases daily
urinary calcium loss by 16 mg. Another way of looking at the effects is:
doubling protein intake from our diet increases the loss of calcium in our
urine by 50%.25
Plant proteins (plant food-bases) do not have these calcium and
bone losing effects under normal living conditions.
Once this
bone material arrives in the collecting systems of the kidney it easily
precipitates into sold formations known as kidney stones.27
Over 90% of kidney stones found in people following a high-protein,
Western diet are formed primarily of bone-derived calcium. Following a
healthy diet is the best way to prevent kidney stones.28
Toxic Sulfur Distinguishes Animal Foods
The qualities of the
proteins we consume are as important as the quantities. One very
important distinction between animal and plant-derived protein is that animal
proteins contain very large amounts of the basic element sulfur.
This sulfur is found as two of the twenty primary amino acids,
methionine and cysteine. Derived from these two primary
sulfur-containing amino acids are several other sulfur-containing amino
acids – these are keto-methionine, cystine, homocysteine, cystathionine,
taurine, cysteic acid.
|
 |
 |
|
Methionine |
Valine |
The yellow sphere represents the element sulfur.

Even though
sulfur-containing amino acids are essential for our survival, an excess of
these amino acids beyond our needs places a critical burden upon our body
and detracts from our health in six important ways:
1) Amino acids, as
the name implies are acids; the sulfur-containing amino acids are the
strongest acids of all, they breakdown into powerful sulfuric acid.
Excess acid, as discussed above, is a primary cause of bone loss leading
to osteoporosis and kidney stone formation.29
2) Methionine is
metabolized into homocysteine – animal foods are the major source of the
amino acid, homocysteine, in people – the more meat in the diet, the
higher a person’s blood level of homocysteine. A diet high in fruits and
vegetables lowers the levels of this amino acid. Epidemiological and
clinical studies have proven homocysteine to be an independent risk factor
for heart attacks, strokes, closure of the arteries to the legs
(peripheral vascular disease), blood clots in the legs (venous
thrombosis), thinking problems (cognitive impairment), and even worse
mental troubles, like dementia, Alzheimer's disease, and depression.30
3) Sulfur feeds cancerous
tumors. Cancer cell metabolism is dependent upon methionine being in the
diet; whereas, normal cells can grow on a methionine-free diet (feeding
off of other sulfur-containing amino acids). This methionine-dependency
has been demonstrated for breast, lung, colon, kidney, melanoma, and brain
cancers.31,32 Increasing methionine in the diet of animals promotes the growth
of cancer.33
There is also evidence of
cancer promoting effects of methionine mediated through a powerful growth
stimulating hormone, called insulin-like growth factor - 1
(IGF-1).34 Meat and dairy products raise IGF-1 levels and promote the
growth of cancers of the breast, colon, prostate, and lung.35
4) Sulfur from sulfur-containing amino acids is known
to be toxic to the tissues of the intestine, and to have deleterious
effects on the human colon, even at low levels.36 The
consequence of a diet of high-methionine (animal) foods may be a
life-threatening inflammatory bowel disease, called ulcerative colitis.37-38
5) Sulfur restriction prolongs life.39 Almost seventy
years ago, restricting food consumption was found to prolong the life of
animals by changing the fundamental rate at which aging occurs.40
Restriction of methionine in the diet has also been shown to prolong the
life of experimental animals. By no coincidence, a diet based on plant
foods is inherently low in both calories and methionine – thus the easiest
and most effective means to a long and healthy life.
6) Possibly a stronger motivation to keep protein,
and especially methionine-rich animal protein, out of your diet is foul
smelling odors – halitosis, body odor, and noxious flatus – akin to the
smell of rotten eggs – are direct results of the sulfur (animal protein)
you eat.41,42
Do Not Waste Your Health Away
Animal foods, full of protein waste, promote poor health
and early death by accelerating the aging process and increasing the risk
of diseases, like heart disease, diabetes, and cancer, that in their own
right, cause premature death. From now on, think of the excess protein
you consume as garbage that must be disposed of in order to avoid toxic
waste accumulation. Obviously, the best action is to avoid the excess in
the first place and this is most easily accomplished by choosing a diet
based on starches, vegetables, and fruits. Within a few days of changing
to a healthy diet, most of the waste will be gone and the damaged
tissues will begin healing.
Unfortunately, you will find little support
for such an obvious, inexpensive, and scientifically-supported approach –
especially when the common masses of people worldwide are ignorant of the
truth – most are gobbling down as much protein as they can stuff in their
mouths – and the food industry is supporting this behavior by advertising
their products as “high-protein” and "Atkins-approved" – as if this was somehow good for the
body. This paradox is age-old, and because it is ruled by emotions,
rather than clear thinking, a change in mind-set in your lifetime, should
not be expected.
Two thousand years ago, in this Bible passage, Paul
asked for tolerance between meat eaters and vegetarians (Romans 14:1-2).
“One man’s faith allows him to eat everything, but another man whose faith
is weak, eats only vegetables. The man who eats everything must not look
down on him who does not, and the man who does not eat everything must not
condemn the man who does...” Do not wait for a consensus before you take action.
References:
1) Chittenden, R. H. (1905).
Physiological economy in nutrition, with special reference to the
minimal protein requirement of the healthy man. An experimental study. New
York: Frederick A. Stokes Company.
2) Fire Retardant Treated Plywood:
http://www.nexsenpruet.com/library/docs/NPCOL1_624753_1.pdf
3) Calloway DH. Sweat and miscellaneous
nitrogen losses in human balance studies.
J Nutr. 1971 Jun;101(6):775-86.
4) Hegsted DM.. Minimum protein
requirements of adults. Am J Clin Nutr. 1968 May; 21(5): 352-7.
5) Dole V. Dietary treatment of
hypertension: clinical and metabolic studies of patients on the rice-fruit
diet, J Clin Invest, 1950; 29: 1189-1206.
6) Millward DJ. The nutritional value of
plant-based diets in relation to human amino acid and protein
requirements. Proc Nutr Soc. 1999 May;58(2):249-60.
7) Mazess RB. Bone mineral content of
North Alaskan Eskimos. Am J Clin Nutr. 1974 Sep; 27(9): 916-25.
8) Brenner BM. Dietary protein intake and
the progressive nature of kidney disease: the role of hemodynamically
mediated glomerular injury in the pathogenesis of progressive glomerular
sclerosis in aging, renal ablation, and intrinsic renal disease. N Engl
J Med. 1982 Sep 9; 307(11): 652-9.
9) Meyer TW. Dietary protein intake and
progressive glomerular sclerosis: the role of capillary hypertension and
hyperperfusion in the progression of renal disease. Ann Intern Med.
1983 May; 98(5 Pt 2): 832-8.
10) Hansen HP. Effect of dietary protein
restriction on prognosis in patients with diabetic nephropathy. Kidney
Int. 2002 Jul; 62(1): 220-8.
11) Biesenbach G. Effect of mild dietary
protein restriction on urinary protein excretion in patients with renal
transplant fibrosis. Wien Med Wochenschr. 1996; 146(4): 75-8.
12) Pedrini MT. The effect of dietary
protein restriction on the progression of diabetic and nondiabetic renal
diseases: a meta-analysis. Ann Intern Med. 1996 Apr
1;124(7):627-32.
13) Cupisti A. Vegetarian diet alternated
with conventional low-protein diet for patients with chronic renal
failure. J Ren Nutr. 2002 Jan;12(1):32-7.
14) Bianchi GP. Vegetable versus animal
protein diet in cirrhotic patients with chronic encephalopathy. A
randomized cross-over comparison. J Intern Med. 1993 May; 233(5): 385-92.
15) Abelow B.
Cross-cultural association between dietary animal protein and hip
fracture: a hypothesis. Calcific Tissue Int 50:14-8, 1992.
16) Frassetto LA .
Worldwide incidence of hip fracture in elderly women: relation to
consumption of animal and vegetable foods. J Gerontol A Biol Sci Med
Sci. 2000 Oct;55(10):M585-92.
17) Maurer M.
Neutralization of Western diet inhibits bone resorption independently of K
intake and reduces cortisol secretion in humans. Am J Physiol Renal
Physiol. 2003 Jan;284(1):F32-40.
18) Remer T.
Influence of diet on acid-base balance. Semin Dial. 2000
Jul-Aug;13(4):221-6.
19) Frassetto L.
Diet, evolution and aging--the pathophysiologic effects of the
post-agricultural inversion of the potassium-to-sodium and
base-to-chloride ratios in the human diet. Eur J Nutr. 2001
Oct;40(5):200-13.
20) Remer T. Potential
renal acid load of foods and its influence on urine pH. J Am Diet
Assoc. 1995 Jul;95(7):791-7.
21) Barzel US. Excess dietary protein can
adversely affect bone. J Nutr. 1998 Jun;128(6):1051-3.
22) Maurer M. Neutralization of Western
diet inhibits bone resorption independently of K intake and reduces
cortisol secretion in humans. Am J Physiol Renal Physiol. 2003 Jan;
284(1): F32-40. Epub 2002 Sep 24.
23) Remer T. Potential
renal acid load of foods and its influence on urine pH. J Am Diet
Assoc. 1995 Jul;95(7):791-7.
24) J Pennington. Bowes & Church’s
Food Values of Portions Commonly Used. 17th Ed.
Lippincott. Philadelphia- New York. 1998.
25) Massey LK . Dietary animal and plant
protein and human bone health: a whole foods approach. J Nutr.
2003 Mar; 133(3): 862S-865S.
26) Jenkins DJ. Effect of high vegetable
protein diets on urinary calcium loss in middle-aged men and women.
Eur J Clin Nutr. 2003 Feb;57(2):376-82.
27) Lemann J Jr. Relationship between
urinary calcium and net acid excretion as determined by dietary protein
and potassium: a review. Nephron. 1999; 81 Suppl 1: 18-25.
28) Delvecchio FC. Medical management of
stone disease. Curr Opin Urol. 2003 May; 13(3): 229-33.
29) Remer T. Influence of diet on
acid-base balance. Semin Dial. 2000 Jul-Aug; 13(4): 221-6.
30) Troen AM. The atherogenic effect of
excess methionine intake. Proc Natl Acad Sci U S A. 2003 Dec 9;
100(25): 15089-94.
31) Cellarier E. Methionine dependency
and cancer treatment. Cancer Treat Rev. 2003 Dec; 29(6): 489-99.
32) Epner DE. Nutrient intake and
nutritional indexes in adults with metastatic cancer on a phase I clinical
trial of dietary methionine restriction. Nutr Cancer. 2002; 42(2):
158-66.
33) Paulsen JE. Growth stimulation of
intestinal tumours in Apc(Min/+) mice by dietary L-methionine
supplementation. Anticancer Res. 2001 Sep-Oct; 21(5): 3281-4.
34) Stubbs AK. Nutrient-hormone
interaction in the ovine liver: methionine supply selectively modulates
growth hormone-induced IGF-I gene expression. J Endocrinol. 2002
Aug; 174(2): 335-41.
35) Yu H. Role of the insulin-like growth
factor family in cancer development and progression. J Natl Cancer
Inst. 2000 Sep 20;92(18):1472-89.
36) Levine J. Fecal hydrogen sulfide
production in ulcerative colitis. Am J Gastroenterol. 1998
Jan;93(1):83-7.
37) Roediger W. Sulphide impairment of
substrate oxidation in rat colonocytes: a biochemical basis for ulcerative
colitis? Clin Sci (Lond). 1993 Nov;85(5):623-7.
38) Christl S. Effect of sodium sulfide
on cell proliferation of colonic mucosa. Gastroenterology 1994;
106:A664 (abstr).
39) Zimmerman JA.
Nutritional control of aging. Exp Gerontol. 2003 Jan-Feb; 38(1-2):
47-52.
40) McCay C. The effect
of retarded growth upon length of lifespan and upon ultimate body size.
J Nutr. 1935; 10: 63-79.
41) McDougall J.
Halitosis Is More than Bad Breath . McDougall Newsletter. January
2002 at
www.drmcdougall.com.
42) McDougall J. Bad
Farts? Meat Stinks! McDougall Newsletter. August 2002 at
www.drmcdougall.com.

|